Introduction
Nutrition plays a pivotal role in supporting health and growth throughout the various stages of life. Nutritional needs change as individuals age, responding to physiological and metabolic changes. It is essential to adjust dietary intake to meet the specific requirements of each life stage. Proper nutrition not only promotes optimal growth and development but also helps in preventing chronic diseases and supporting overall well-being. This research provides an in-depth look at the nutritional requirements across different life stages, including infancy, early childhood, adolescence, adulthood, and older adulthood.

1. Nutrition in Infancy (0-2 Years)
Infancy is a critical period for growth and development, where proper nutrition lays the foundation for lifelong health.
Key Nutritional Needs
• Breast Milk or Formula:
• Breast Milk: Ideal for infants, providing all necessary nutrients, antibodies, and fatty acids like DHA, crucial for brain development.
• Formula: A suitable alternative for those not breastfeeding, designed to mimic the nutritional profile of breast milk.
• Macronutrients:
• Proteins: Essential for growth and development of muscles and tissues.
• Fats: Vital for brain development and energy, especially omega-3 fatty acids.
• Carbohydrates: Provide energy; primarily from lactose in breast milk.
• Micronutrients:
• Vitamin D: Important for calcium absorption and bone health.
• Iron: Critical for cognitive development; iron-rich foods can be introduced at six months.
Feeding Practices
• Exclusive Breastfeeding: Recommended for the first six months by the WHO.
• Introduction of Solids: After six months, start with iron-fortified cereals, pureed fruits, and vegetables, gradually introducing more textures.
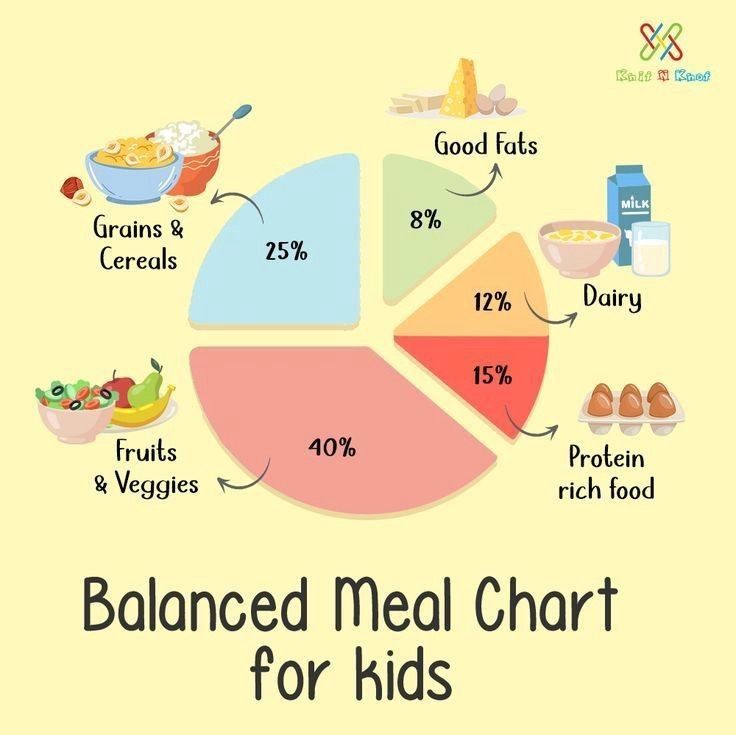
2. Nutrition in Early Childhood (2-6 Years)
During early childhood, nutritional needs support continued growth, cognitive development, and physical activity.
Key Nutritional Needs
• Energy and Macronutrients:
• Increased Caloric Intake: Necessary due to high activity levels.
• Balanced Macronutrients:
• Proteins: Supports growth and development.
• Healthy Fats: Crucial for brain development.
• Carbohydrates: Primary energy source.
• Vitamins and Minerals:
• Calcium and Vitamin D: Essential for bone health.
• Iron: Prevents anemia and supports growth.
• Fiber: Supports digestive health.
Feeding Practices
• Balanced Diet: Focus on a variety of fruits, vegetables, whole grains, lean proteins, and dairy.
• Healthy Snacks: Offer nutritious snacks like fruits, vegetables, and whole-grain options.
• Limit Sugary Foods: Reduce intake of processed and high-sugar foods to prevent obesity and dental issues.

3. Nutrition in Adolescence (12-18 Years)
Adolescence is marked by rapid growth and hormonal changes, necessitating increased nutritional intake.
Key Nutritional Needs
• Proteins: Essential for muscle growth and tissue repair during growth spurts.
• Calcium and Vitamin D: Critical for achieving peak bone mass.
• Iron: Increased requirements, especially for menstruating females.
• Folic Acid: Important for cell growth and development, particularly for females.
Feeding Practices
• Increased Caloric Needs: Emphasize nutrient-dense foods to meet higher caloric demands.
• Variety of Foods: Encourage consumption of whole grains, fruits, vegetables, and lean proteins.
• Healthy Lifestyle: Promote regular physical activity alongside a balanced diet to support healthy growth.
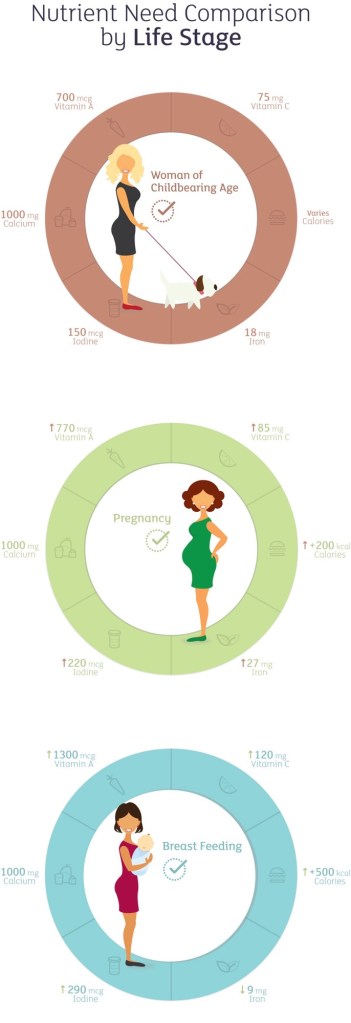
4. Nutrition in Adulthood (19-50 Years)
Adulthood focuses on maintaining health, preventing chronic diseases, and supporting an active lifestyle.
Key Nutritional Needs
• Macronutrients:
• Proteins: Important for muscle maintenance and metabolic functions.
• Healthy Fats: Omega-3 fatty acids support cardiovascular health.
• Carbohydrates: Focus on whole grains for energy and fiber.
• Vitamins and Minerals:
• Calcium and Vitamin D: Essential for bone health.
• Antioxidants: Vitamins C, E, and beta-carotene protect against cellular damage.
• Iron: Supports energy metabolism and oxygen transport.
Feeding Practices
• Balanced Diet: Prioritize a variety of whole foods, including fruits, vegetables, lean proteins, and whole grains.
• Portion Control: Maintain appropriate portion sizes to manage weight.
• Hydration: Adequate water intake supports overall health and metabolic processes.

5. Nutrition in Older Adulthood (50+ Years)
As people age, metabolic rates decline, and nutritional needs shift to maintain health and prevent age-related diseases.
Key Nutritional Needs
• Proteins: Essential for maintaining muscle mass and preventing sarcopenia.
• Calcium and Vitamin D: Critical for bone density and health.
• Vitamin B12: Absorption decreases with age, necessitating dietary adjustments or supplementation.
• Fiber: Supports digestive health and prevents constipation.
• Hydration: Increased risk of dehydration due to diminished thirst perception.
Feeding Practices
• Small, Frequent Meals: Easier to digest and helps in managing energy levels.
• Nutrient-Dense Foods: Focus on foods high in vitamins and minerals to prevent deficiencies.
• Supplementation: Consider vitamins and minerals that may be lacking in the diet, especially calcium, vitamin D, and B12.
Conclusion
Nutritional needs evolve throughout life, reflecting changes in growth, metabolism, and health status. Meeting these needs with a balanced, nutrient-rich diet is essential for promoting health and preventing disease at every age. From the rapid growth of infancy to maintaining health in older adulthood, proper nutrition plays a foundational role in ensuring a healthy and fulfilling life.
References
1. World Health Organization (WHO). Healthy Diet. 2022.
2. National Institute on Aging (NIA). Nutrition as You Age. 2021.
3. American Academy of Pediatrics (AAP). Infant Nutrition and Feeding. 2020.
4. Academy of Nutrition and Dietetics (AND). Nutrition Across the Lifespan. 2021.
5. Mayo Clinic. Healthy Eating for Adolescents. 2022.
6. Centers for Disease Control and Prevention (CDC). Nutrition for Older Adults. 2021.

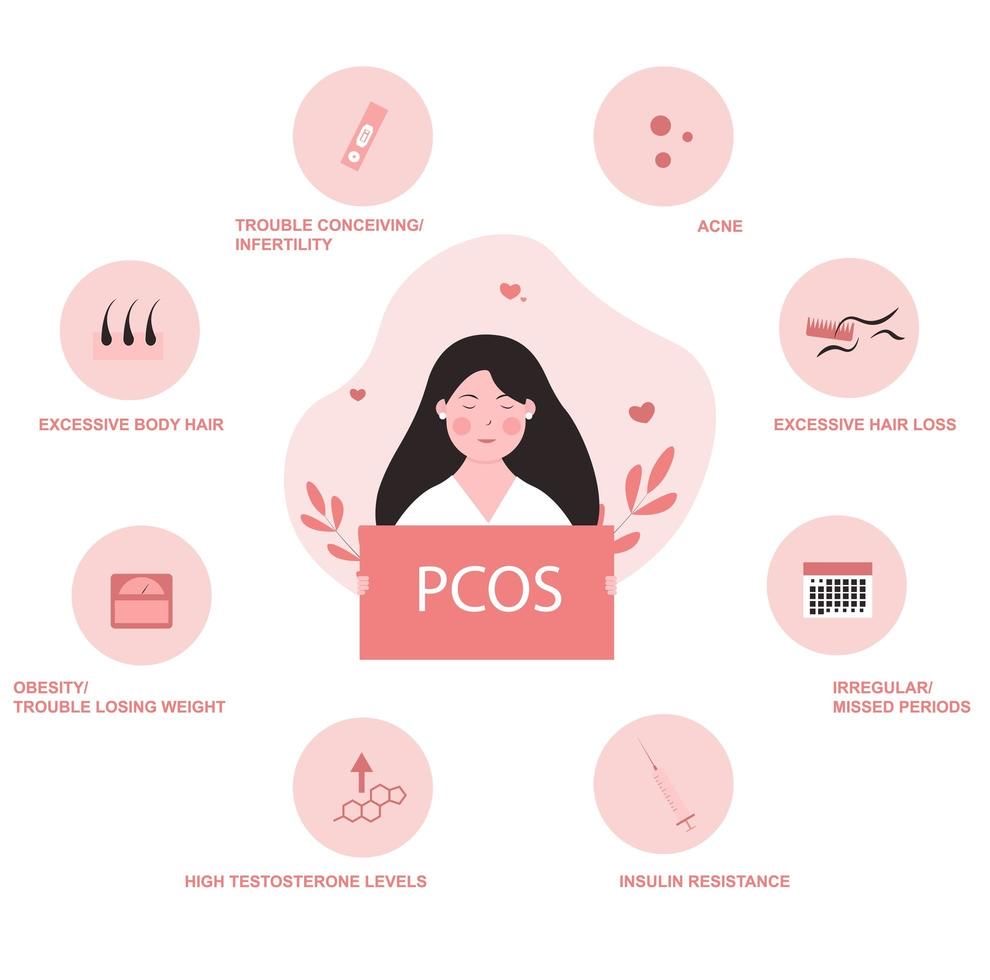
 Type 2 Diabetes Mellitus (T2DM)
Type 2 Diabetes Mellitus (T2DM)