1. Insulin Resistance (IR)

Insulin resistance occurs when the body’s cells don’t respond properly to insulin, the hormone that helps regulate blood sugar levels. As a result, the pancreas produces more insulin to compensate. This elevated insulin (hyperinsulinemia) is linked to several metabolic disorders, including PCOS and T2DM. Insulin resistance affects 10-25% of the general population, particularly in those who are overweight or obese.
2. Polycystic Ovary Syndrome (PCOS)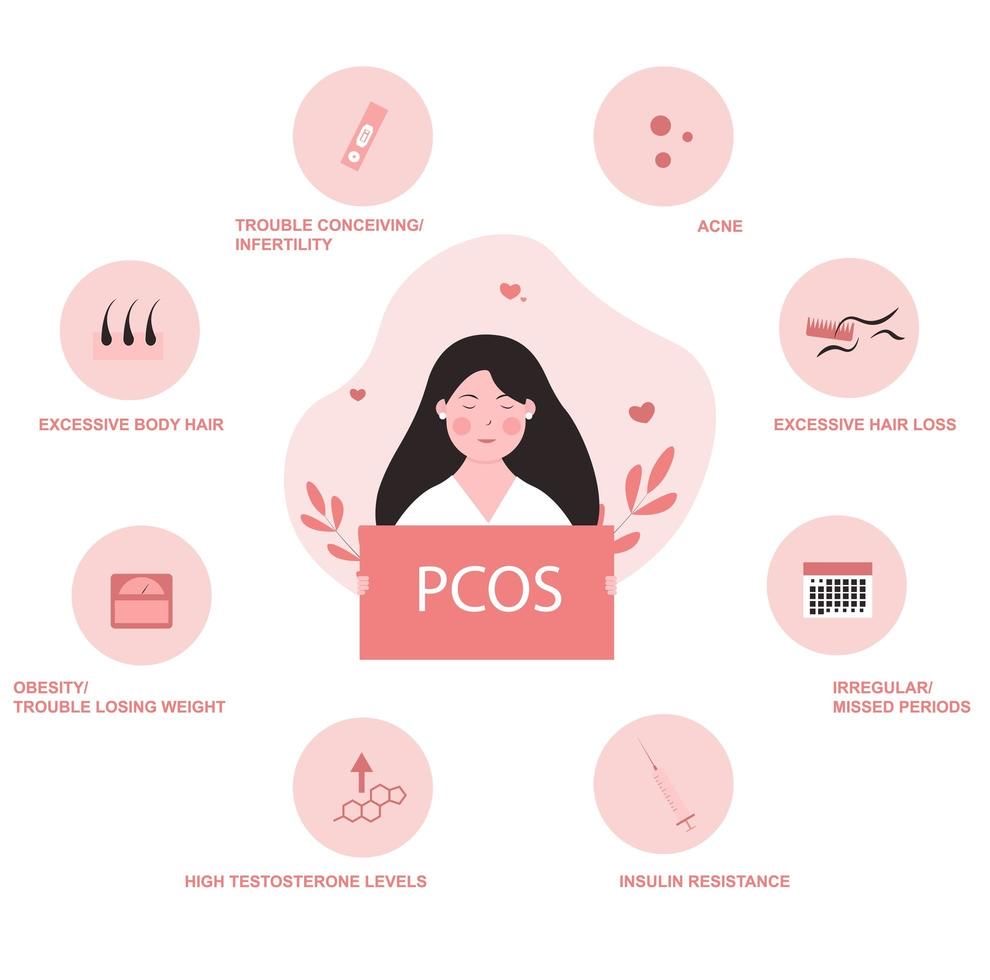
PCOS is a hormonal disorder that affects 4-6% of reproductive-aged women, characterized by excess androgen (male hormone) production, irregular ovulation, and the presence of multiple cysts on the ovaries.
• Link to Insulin Resistance: Up to 50-70% of women with PCOS have insulin resistance, even if they are not overweight. Insulin resistance in PCOS leads to elevated insulin levels, which further stimulates the ovaries to produce more androgens (like testosterone), worsening symptoms such as acne, excessive hair growth (hirsutism), and irregular menstrual cycles.
• Reproductive Impact: The excess androgens interfere with ovulation, leading to infertility in many women with PCOS. The hormonal imbalance caused by insulin resistance is central to this dysfunction.
3.  Type 2 Diabetes Mellitus (T2DM)
Type 2 Diabetes Mellitus (T2DM)
T2DM is a chronic metabolic disorder where the body either doesn’t produce enough insulin or is unable to use it effectively. Over time, the pancreas becomes unable to keep up with the demand for insulin, leading to high blood glucose levels.
• Prevalence and Link to PCOS: Between 80-100% of individuals with T2DM exhibit some degree of insulin resistance. Women with PCOS are 5-10 times more likely to develop T2DM compared to women without PCOS. This is because both conditions are linked to insulin resistance and hyperinsulinemia.
• Progression to Diabetes: Around 30% of women with PCOS may have impaired glucose tolerance (IGT), a precursor to T2DM, and 10-20% may eventually develop full-blown diabetes, especially as they age.
4. The Bi-directional Relationship Between PCOS and T2DM
• PCOS Increases Risk of T2DM: The hyperinsulinemia seen in PCOS not only leads to reproductive issues but also significantly increases the risk of developing glucose metabolism disorders like IGT and T2DM. Studies have shown that up to 10% of women with PCOS between the ages of 25-35 already have T2DM, and the percentage increases with age.
• T2DM Increases Risk of PCOS: Although less studied, there is growing evidence that women with T2DM are more likely to exhibit symptoms of PCOS. One study found that 26% of reproductive-aged women with T2DM had PCOS, compared to only 4-6% in the general population.
6. Clinical Consequences and Long-Term Risks
• For PCOS: In addition to reproductive issues like infertility and irregular periods, women with PCOS are at a higher risk for metabolic syndrome, which includes central obesity, dyslipidemia (high cholesterol/triglycerides), and hypertension (high blood pressure). This significantly increases the risk of cardiovascular diseases.
• For T2DM: T2DM, if unmanaged, leads to long-term complications such as cardiovascular disease, nerve damage (neuropathy), kidney damage (nephropathy), eye problems (retinopathy), and an increased risk of stroke.
• For Both Conditions: Since insulin resistance plays a key role in both PCOS and T2DM, women who suffer from one condition should be regularly screened for the other. PCOS increases the risk of developing T2DM, while women with T2DM are more likely to develop PCOS-like symptoms due to elevated insulin levels.
7. Treatment Approaches
• Lifestyle Modifications: Weight loss, exercise, and dietary changes are first-line treatments for both PCOS and T2DM, as they help improve insulin sensitivity and reduce the risk of complications. Even modest weight loss (5-10% of body weight) can significantly improve insulin sensitivity and reduce PCOS symptoms.
• Medications:
• Metformin: Commonly used in T2DM to improve insulin sensitivity, metformin is also effective in treating insulin resistance in women with PCOS. It can help regulate menstrual cycles, improve ovulation, and reduce androgen levels.
• Thiazolidinediones (TZDs): These insulin-sensitizing agents can also be used to treat both T2DM and PCOS, though they are less commonly prescribed due to side effects.
• Oral Contraceptives: For women with PCOS, hormonal birth control is often prescribed to regulate menstrual cycles, reduce androgen levels, and improve symptoms like acne and hirsutism.
• Anti-androgen Medications: Drugs like spironolactone can be used to block the effects of androgens in PCOS patients.
8. Research Directions
Recent studies are investigating whether PCOS and T2DM represent different phenotypes of the same underlying insulin resistance syndrome. Understanding the specific molecular mechanisms of insulin resistance in these disorders may lead to better targeted treatments in the future.
Conclusion:
Both PCOS and T2DM are metabolic disorders linked through insulin resistance. While they present differently—PCOS with reproductive and hormonal issues and T2DM with glucose metabolism dysfunction—their underlying cause is often the same. Women with PCOS are at a higher risk of developing T2DM, and women with T2DM may also exhibit signs of PCOS. Understanding the interplay between these conditions is crucial for effective treatment and management to prevent long-term health complications.
Very nice topic, well done for publishing. I would like to share some information with you.
1. Low-Carbohydrate Diet
This type of diet helps stabilize blood sugar levels and reduce insulin spikes.
• Recommended Foods:
• Non-starchy vegetables (such as broccoli, spinach, lettuce, and cauliflower).
• Lean proteins (chicken, fish, lean meats).
• Healthy fats (olive oil, avocado, nuts).
• Eggs.
• Low-fat or unsweetened dairy products.
• Foods to Limit:
• Refined carbohydrates (white bread, pasta, white rice).
• Sweets and added sugars.
2. Low-Glycemic Index (Low-GI) Diet
Low-GI foods release sugar slowly into the bloodstream, helping stabilize blood sugar and insulin levels.
• Recommended Foods:
• Whole grains (oats, quinoa, barley).
• Fresh fruits (berries, apples, pears).
• Leafy green vegetables.
• Legumes (lentils, beans, chickpeas).
• Nuts and seeds.
• Foods to Avoid:
• Sugary drinks.
• Pastries and sugary snacks.
• Potatoes and white rice.
3. Mediterranean Diet
This diet is considered one of the healthiest, emphasizing healthy fats and plant-based proteins.
• Recommended Foods:
• Fresh fruits and vegetables.
• Fatty fish (like salmon and tuna).
• Olive oil.
• Nuts and seeds.
• Whole grains.
• Legumes.
• Foods to Avoid:
• Processed red meats.
• Fried foods and unhealthy fats.
4. Plant-Based or Semi-Vegetarian Diet
A plant-based diet is rich in anti-inflammatory foods and can help improve insulin sensitivity.
• Recommended Foods:
• Fresh and cooked vegetables.
• Whole grains.
• Fruits.
• Nuts and seeds.
• Legumes.
• Foods to Avoid:
• Processed and packaged foods with additives.
• Sugary snacks and foods high in sugar.
5. Sample Daily Meals:
Breakfast:
• Option 1: Oatmeal with apple slices, cinnamon, and some nuts.
• Option 2: Veggie omelet with leafy greens and olive oil.
Lunch:
• Option 1: Large salad with grilled chicken, avocado, and fresh vegetables, dressed with olive oil and lemon juice.
• Option 2: Grilled salmon with quinoa and roasted vegetables.
Dinner:
• Option 1: Grilled chicken breast with roasted broccoli and cauliflower.
• Option 2: Lentil soup with a side salad.
Snacks:
• A handful of nuts.
• Low-sugar fruits (like berries).
• Unsweetened Greek yogurt.
6. Additional Tips:
• Fiber: Include fiber-rich foods like leafy greens and legumes to improve insulin sensitivity.
• Added Sugar: Avoid sugary foods and drinks, as they worsen insulin resistance.
• Protein: Make sure to have protein with each meal to help regulate blood sugar and keep you full longer.
Conclusion: A diet rich in protein and fiber, while low in refined carbohydrates and added sugars, is ideal for managing insulin resistance and PCOS.
LikeLiked by 1 person
Good topic and great work on this topic, I will add information I know.
Shared Insulin Resistance Pathways: Insulin resistance is the common denominator in both PCOS and T2DM. In PCOS, insulin resistance predominantly affects glucose transport and lipid metabolism in fat cells, leading to increased androgen production in the ovaries. In T2DM, insulin resistance primarily affects muscle, liver, and fat tissue, leading to glucose intolerance and elevated blood sugar levels.
Androgen Excess and Insulin Resistance: In PCOS, high insulin levels stimulate the ovarian theca cells to produce more androgens. Androgens exacerbate insulin resistance, creating a vicious cycle. Moreover, high insulin levels reduce the production of sex hormone-binding globulin (SHBG), increasing the amount of free androgens, which worsens symptoms.
Genetic and Environmental Factors: Both conditions share common genetic factors that increase susceptibility to insulin resistance. Obesity, diet, and physical inactivity can further exacerbate both PCOS and T2DM. However, even lean women with PCOS can have significant insulin resistance, indicating a genetic predisposition.
LikeLike